Abstract
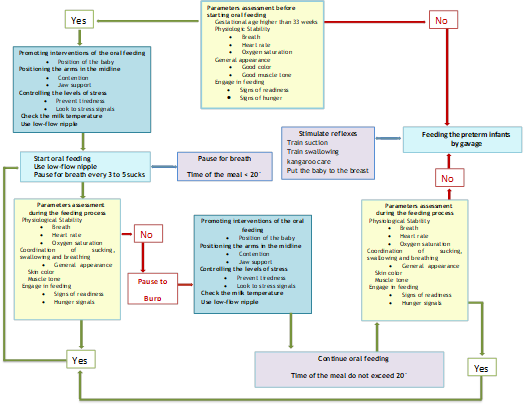
The transition from tube feeding, to oral feeding is one of the most difficult for preterm infants. It’s a continuous but slow process, which demands physiological development respiratory independence and the ability to coordinate suction, breathing and swallowing. Getting the premature to develop his/her feeding skills is the big challenge to the professionals that work in the NICU. Objectives: To know the characteristics of preterm infants, essentials for oral feeding; to know the nurses’ opinion on nursing interventions, that promote the transition of gavage feeding for oral feeding in preterm infants; to contribute to the development of a proposal for a guide to oral feeding in preterm infants. Methodology - Qualitative, exploratory and descriptive study. Semi-structured interviews were performed to neonatal nurses. Content analysis to treat data was used. Results - Weight, gestational age, physiological stability, sucking coordination, swallowing and breathing, and feeding involvement, are fundamental parameters to begin oral feeding. Positioning the baby, reflexes stimulation, control stress levels, monitoring the temperature and the milk flow, are nursing interventions that promotes the development of feeding skills. The existence of a guide not only gives security but also promotes the respect for the developmental stages of the preterm infant, the standard of care, encourages learning, reduces the subjectivity and fosters the evidence based practice, nevertheless, it ought to have a simple structure, be practical/judicious and small. Conclusion: An algorithm for the preterm infants oral feeding was developed grounded on nurses’ opinion but also in the best available evidence.
Keywords: Preterm infants, feeding skills, swallowing, sucking
Introduction
Technological innovation has been a concern in modern societies, reflected in the quality of care. Aspects such as mortality and morbidity have been declining significantly, particularly in the field of neonatology, where we verify a higher survival rate of infants with gestational age increasingly low. Every year about one in every eight children born before 37 weeks of gestation (early) may require intensive care in the first days, weeks or months of his life (Briere [et al.] 2014).
The technology developed in the past decades has contributed to saving lives outside the intrauterine environment, even the most premature infants (Als, 2004; Alana,&Timothy, 2012). In the last years there has been an intense development in the care of newborns, especially premature babies (Cheong and Doyle, 2012) contributing to a drastic reduction of infant mortality (INE, 2014).
With the increased survival of premature infants, there is the perception that the difficulty in feeding is an important milestone that these children need to overcome (Crowe, Chang and Wallace, 2012; Fucile [et al.], 2012). Most term newborns are born with skills for oral feeding, however, this is not the case of premature babies, who are known to have difficulty in making the gavage feeding transition to oral feeding (Lau, Smith, Schanler, 2006; Bingham [et al.], 2012).
The sensory and motor immaturity, with the restriction of experiences during a critical period of brain development when the pre-power skills are refined, are factors that potentiate significant delays in the emergence of food skills of premature newborns (Barlow [et al .], 2010).
Professionals recognize the immaturity in sucking, swallowing, breathing and coordination among the three factors are the main causes for the delay of the clinical discharge of these babies (Stumm [et al.] 2008; Bingham, 2011).
The difficulties inherent in the establishment of skills for oral feeding, associated with additional prolonged hospitalization costs and increased stress in parents, bring out the need to develop and evaluate therapeutic tools that facilitate the normal development of oral motor skills of premature babies (Lau, 2006 Barlow [et al.], 2008; Bauer [et al.], 2009; Medeiros [et al.], 2010).
Effective interventions, to improve premature baby feeding performance as early as possible in order to prevent eating disorders in childhood, are needed (Fucile [et al.], 2011); (Bingham [et al.], 2012; (Fucile [et al.], 2012).
It is the responsibility of nurses to observe the communication signals, biological and behavior of the child, to make their decisions and help premature infants to acquire the skills for efficient oral feeding (Lau, Smith, Schanler, 2006; Ross, & Philbin, 2011), demands the need to study the transition to oral feeding in preterm infants. Therefore, we conducted a research which problem was: How to improve the transition from gavage feeding for feeding to oral feeding in premature infants? and the aims were:
- To know the characteristics of preterm infants in the opinion of nurses are key to oral feeding;
- To know the opinion of nurses on the nursing interventions, which they consider that promote the transition from gavage feeding to oral feeding in premature infants;
- To contribute to the development of a proposal for a guide to start oral feeding in preterm infants.
Reducing the length of hospitalization of premature newborns, through nursing interventions that promote the transition to oral feeding, as well as representing significant gains in health, also contributes to improve the quality of the feeding in childhood.
Methods
A qualitative, exploratory and descriptive study was conducted and the participants were nurses from the neonatal unit of Hospital de São João EPE (CHSJ) of Porto – Portugal. The inclusion criteria to select the participants were: nurses with the specialization in child health and pediatrics and more than three years of professional exercise in neonatology. The exclusion criteria were: nurses with management functions in the neonatology; nurses being trained in the (NIDCAP); nurses being trained in the (EFS).
Several semi-structured, face to face interviews were performed and recorded in an audio device and then content analysis was used to treat data.
The interview guide was developed with three open questions such as:
- Which are the characteristics of preterm infants that, in your opinion, are fundamental to the oral feeding?
- What is your opinion on nursing interventions that promote the transition to oral feeding of the preterm infants?
- What do you think about the existence of a guideline for oral feeding in preterm infants?
The script was validated by conducting a pre-test, a nurse who met similar characteristics to the participants in order to assess whether the issues would be easily understandable and allow the collection of relevant information.
Interviews were conducted in the Neonatology unit of CHSJ from March to June 2013. Their achievement was dependent on the availability of each participant. Interviews were conducted in an appropriated and calm environment, ensuring privacy and safeguarding the anonymity of the participants and we also requested their permission to audio record the interviews. The interviews were coded with the letter E, followed by a number corresponding to the order recorded, E2 to E11. After transcribing the interviews, its contents were validated with participants and then the recordings destroyed.
Findings and Discussion
The content analysis was carried out in three stages, "pre analysis", "exploitation material" and finally the "treatment of the results: inference and interpretation." Three themes emerged, such as:
"Evaluation parameters of preterm infants for oral feeding"; "Nursing interventions promoting the transition to oral feeding of premature newborn" and "Nurses’ opinion on the existence of a guideline for oral feeding of preterm infants."
The theme "evaluation parameters of preterm infants for oral feeding" allows a better understanding of the views of nurses on the physical as well as physiological and behavioral changes, manifested by the baby and that act as decision criteria, for oral feeding in preterm infants.
The category "The weight"
Some nurses consider the baby's weight, an important feature to take into account at the time of starting oral feeding. However, there was no consensus on the minimum weight to start oral feeding in preterm infants.;
The category "gestational age"
Nurses considered that from 33 weeks if the baby shows interest should start oral feeding, for them infants with very low gestational age, do not have skills because of the lack of maturity that do not allow them to coordinate sucking and swallowing with breathing.
The category "physiological stability"
This category includes three subcategories: "Breath"; "Heart Rate" and "Oxygen Saturation."
The subcategory "Breath"
Nurses are of the opinion that food requires an expense increased energy, so it is necessary that the baby is stable at physiological level and respiratory independence, so he/she will be able to perform this task without the expense of other more important.
The subcategory
It was also noted that a premature baby in nasal Continuous Positive Airway Pressure (CPAPn), should not be fed spontaneously, and must be independent, clinically well and with stable vital signs. They considered it essential to assess the baby's behavior, respect respiratory stability and let him/her be the major driver of oral feeding.
Furthermore, it was noted that, although the respiratory independence is important, there are characteristics such as pulmonary dysplasia, with which the premature infant can live comfortably with stable respiratory conditions.,
The subcategory
It was referred only by a participant, however the importance of its role in physiological stability of the premature baby cannot be underestimated.
The subcategory "Oxygen saturation”
It was considered a parameter to take into account for the oral feeding in premature baby.
The O2 saturation were considered by participants as an indicator of physiological stability, as well as other vital signs [heart rate and breathing], because it is directly related to the baby good performance during oral feeding.
The category "coordination of sucking, swallowing and breathing"
The coordination of these factors was considered as an essential feature to start oral feeding safely Nurses are of the opinion that the swallowing itself, coordination of sucking, swallowing and breathing is included, to be made in a safe way. Also report that the baby does not have the coordination of three factors [sucking, swallowing, breathing], however, how much you insist, he/she is unable to feed safely and efficiently. They consider that the sucking reflex in premature baby can be searched offering a few drops of milk or sucrose and verify if they can coordinate sucking, swallowing and breathing. They are of the opinion that a premature baby who seeks the teat with reflection of very present and powerful suction, shows signs of maturity and stability to begin oral feeding.
The category "General Appearance"
The overall look can be identified by the physical and behavioral characteristics of the baby. The good general aspect refers to the premature newborn who has a pink color of the skin, good vitality and good muscle tone.
In this category were identified two subcategories: "skin color" and "muscle tone".
The color of the skin can be a strong indicator of the stability of the premature newborn and hence its ability to initiate, in a safe, oral feeding.
Nurses gave relevance to the color of the skin, particularly the pallor, considered a disability indicator for oral feeding.
The subcategory "Muscle tone"
It seems to be directly related to the strength of the baby.
For this subcategory, the nurses are of the opinion that a baby who is active and with force is a baby who has more power to start oral feeding. If on the other hand, do not show interest in breastfeeding, is sleepy, hypotonic and without force, then does not have the necessary conditions to begin oral feeding.
The category "Involvement in feed"
It refers to the interest showed by the baby to suckle spontaneously. In this category emerge two subcategories: "Signs of readiness" and "Hunger signals".
The subcategory "signs of readiness"
Refers to the movements of the extremities and head, how to get hands to his/her face and mouth, sucking movements and calm state of alert.
The subcategory "hunger signals"
It refers to the premature baby's behavior, when he/she moves the extremities and the head, moves his/her hands in the face or mouth, moves his/her face against the bedclothes, with sucking movements and behavioral state of excitement and tears.
In the participants’ opinion, a baby is hungry when he/she is awake, crying, features a strong suction, with movements of the head in search of the teat, meaning that it is dissatisfied, hungry and wants to feed spontaneously.
The second theme brings together the views of nurses on the nursing interventions that they considered that promote the development of food skills of the premature newborn.
Five categories and several subcategories emerged such as: "position the baby" (alignment in the midline, containment, jaw support); "Stimulate the reflexes" (train sucking, swallowing training, running technique kangaroo care, putting baby to the breast); "Control levels of stress" (prevent fatigue, stress observe signs); "Monitor the temperature of the milk" and "feed the baby with low-flow teat",
The category “Positioning the baby”
Position the baby during the feeding is an intervention extremely important to the success. From this category emerged subcategories such as: "alignment in the middle line," "containment" and "jaw support."
The subcategory "alignment in the middle line" refers to the baby's position, they consider ideal when being fed orally. Nurses consider to take the baby in her lap, wrapped and positioned sideways, with members in the midline so that light hand to mouth is the ideal position to start oral feeding and is therefore, an intervention that promotes skills development.
The subcategory "containment" refers to the involvement of the baby with a cloth diaper, to maintain a position aligned with the limbs in flexion, preventing uncoordinated movements, as described by the following units: To take the baby in the nurses’ arms, wrapped and contained in a diaper is a positioning warmth and comfortable, which provides security, coordination and self-regulation at the time of feeding.
The subcategory "jaw support" emerges from the same category, since the participants considered the support and stabilization of the jaw, as a support measure to immature baby skills and a means of promoting self-regulation.
The category "Stimulate the reflexes"
Refers to measures used by nurses, in stimulating the necessary reflexes which are engaged in the process of the premature oral feeding. From this category also emerged subcategories such as: "train suction", "train swallowing", "run Kangaroo care technique" and "put the baby to the breast.
The subcategory "train suction" refers to the set of interventions that, in the opinion of nurses are needed to train the sucking reflex.
Nurses consider that promoting non-nutritive sucking is essential to help the premature baby to develop the sucking reflex.
The subcategory "Training swallowing" refers to the measures taken by nurses to develop the swallowing reflex.
Help the premature baby to train swallowing implies to help the coordination between swallowing and breathing. Thus, nurses consider that offering the teat with a few drops of milk or sucrose, while feeding by tube, promotes the development of food skills of premature baby. This experience has an effect on changes in the number of sucks and swallowing, and can therefore result in his/her early ripening.
The subcategory "do Kangaroo care " refers to a measure adopted by nurses in order to stimulate the reflexes.
Nurses are of the opinion that Kangaroo care method is a facilitative intervention to the stimulation of reflexes, since the contact skin to skin stimulates the production of milk, gives the baby the opportunity to feel the breast, smell the milk and smell the mother, while being tube fed.
The subcategory "put the baby to breast" refers to the fact that preterm infants be placed in the breast while being tube fed, help to stimulate the reflexes.
The nurses considered to place the baby on the breast while it is fed by gavage, is a form of stimulation of breast milk on the one hand, and on the other side is a form of stimulation of sucking and swallowing reflexes.
The category "Control the levels of stress"
Refers to the attitudes that nurses have about the baby before and during the meal in order to avoid as much stress which may involve oral feeding. From this category emerged subcategories such as "prevention fatigue" and "observe stress signs."
The subcategory "prevention fatigue" includes the registration units where nurses express their opinion on the measures that are important in the prevention of fatigue, including the organization of care before starting oral feeding.
Reduce the stimulus, respect the pauses between sucks, observe the stress signals of the baby and prevent fatigue, in order to conserve energy, are interventions that promote the development of food skills in the premature baby. Nurses consider important to note the premature baby's behavior and understand it through the signs that he/she manifested, know when to stop, give them support when they manifest signs of fatigue, drowsiness, physiological or intolerance stimulation instability, helping their self-regulation.
The subcategory "observe signs of stress" refers to the observation of signs of discomfort or instability of preterm infants during the process of oral feeding.
The child's ability to eat is directly related to the nurse's ability to understand and be sensitive to respond to physiological and behavioral baby communication, helping them to achieve a quality food.
The category "Check milk temperature "
Refers to the suitable temperature of the milk at the time of feeding.
Check the milk temperature was considered by the nurse, an important measure for the baby's performance during feeding.
The category refers to a measure that allows the newborn to remain stable, from a physiological point of view, and organized, the neuro-behavioral point of view, to be fed with a suitable milk flow to maturity.
On this topic it can be concluded that nurses consider that the timing of food must be carefully prepared, in a calm and relaxing environment, taking into account the baby fatigue and stress signs.
Nurses considered that the stimulation of reflexes can be done in a pleasant way by placing the baby on the breast, making Kangaroo care or providing non-nutritive sucking.
The alignment with restraint to the midline and jaw support were considered indispensable measures in support of self-regulation and the baby concentration during the meal.
A teat low flow and a proper temperature milk appear to give the baby a learning opportunity and also a time of comfort and pleasure.
The third theme refers to the existence of a guiding tab of oral feeding in preterm infants. Nine categories emerged such as: "Gives security"; "Reduces subjectivity"; "Promotes respect for developmental stages"; "Promotes standard of care"; "Promotes the partnership of care"; "Reduces the length of stay"; "Encourages the training"; "Promotes evidence-based practice" and "Characteristics of a guide" (simple, small, practical / careful).
The category "Gives security"
The nurses consider the possibility of a guiding tab gives safety in the care of the premature baby. "... In terms of safety ... if you can make an observation based on those parameters ... first do not lose you so much ... and you end up having a mindset that maybe nothing escapes you the level of essential have is to evaluate ..." E7
The categoryshows that the existence of a guide will help nurses to evaluate the premature baby with rigor and objectivity in the process of transition to oral feeding.
The category "It promotes respect for the developmental stages"
The existence of a guide will contribute to respect the pace and characteristics of the premature baby.
The recognition of the developmental process of physiological subsystems, motor and neurological as well as influence the current feeding practices in preterm infants, allows professionals and parents to help the child to have more organized food experiences.
The category “Promotes standard of care"
This category emphasizes that the existence of a guide may be a means to promote standardization of care, following the same guideline.
The category "Promotes the partnership in care"
This category reveals the need for partnership between professionals and parents, characterized by their presence and involvement in care.
Nurses consider that the existence of a guide would help them regarding the parents’ education performed by different people. Will also allow nurses to help parents to be the best caregivers because they can better understand the baby and identify warning signs.
The category "Decreases the length of stay"
Revealed in partycipants’ opinions that the existence of a guide could help to reduce the premature baby's hospital stay in the NICU.
The category "It encourages the training"
Reveals that access to training in this area, enabling direct nurses to determine when to start oral feeding.
The category “Promotes evidence-based practice”
Refers to the need for a systematic and continuous updating of scientific knowledge, by professionals on the complex process of premature infant feeding.
The category "Characteristics of a guide"
In this category there are three subcategories: "Simple"; "Little"; "Practical / judicious."
The subcategory "Simple", nurses consider that the guide should be clear, with a few items, easy to apply.
The subcategory "Little"
Nurses consider that a guide should be rather extensive, in order to facilitate the reading. "... A guide, who was not a complicated guide, I do not think I need to have many items ...”E8
The subcategory "Practical / judicious"~
A guide should be small, simple and practical / judicious, with protocols and criteria set to start oral feeding in premature baby. Not a sealed document but one guideline.
Nurses referred that a guide would be a key tool for communication among professionals, a resource in the promotion of partnership care and a means to standardize practices. It should be based on rigorous and objective parameters. This would be the ideal instrument to promote evidence-based practice and a way to promote scientific bases on the baby's development stages, avoiding act on free will.
Conclusions
Through the opinions of nurses working in neonatology, and who agreed to participate in this study, it was possible to access data that give a broader view on the start of oral feeding to premature babies.
Before starting oral feeding, it is essential to evaluate some parameters without which this process would be compromised with certainty.
There was no consensus on nurses’ opinion regarding the minimum weight of the premature newborn to begin oral feeding, however, regarding gestational age it should not be less than 33 weeks. These parameters are directly related to the suction force and the maturation of food skills, without which the child would be unable to perform this task.
The physiological stability in general and in particular respiratory independence, heart rate and oxygen saturation within the proper parameters were considered prerequisites for coordination capacity of sucking and swallowing with breathing of preterm infants.
Without the presence of suction reflexes and swallowing, and more specifically the coordination between them and breathing, the premature infant would be unable to feed spontaneously and with the risk of compromising the physiological stability by incoordination oro motor.
The general appearance such as the staining of the skin and muscle tone are indicators which cannot be disregarded. These parameters translate the clinical condition of the baby and hemodynamic stability, which are essential for the premature bay actively participate with vitality and vigor at the time of supply, without unnecessary energy expenditure. This requires from the baby readiness and hunger signals. The baby must be awake, looking for the teat, present a strong suction and will suck. A baby who does not show interest, is hypotonic or sleeping idly without signs of readiness, should be fed by tube. The positioning of the baby contained, aligned to the midline, contributes to stay focused and self-regulated.
A baby who is quiet and awake, showing interest, which is concentrated and focused to perform their new skill, means that is involved in feeding.
The stimulation of reflexes was also considered important in the development of food skills of premature baby. There were several forms of stimulation of reflexes, referred by nurses: train sucking and swallowing by non-nutritive sucking with a pacifier and a few drops of sucrose or a few drops of milk and put the baby to breast and kangaroo care.
Attitudes before and during the meals are determining factors in the baby's ability to maintain the organization and self-regulation necessary for their good performance. The organization of nursing care before the meal, such as changing the diaper, bathing or aspiration of secretions should be carefully planned to preserve energy for the difficult task of oral feeding.
The stress signals expressed by preterm infants during the meal, such as turning the head back, change in skin color, oral peri pallor, drowsiness, polypnea, uncomfortable facies, according to the nurses, are indicators that are essential to stop, let the baby rest and give him/her the necessary support to its self-regulation. Respect breaks between each outbreak of three to five sucks gives time for the baby to breathe, maintain physiological stability and prevent fatigue.
The decrease of stimuli, such as light intensity and the noise around the baby protects it from stress factors and promotes their involvement in the feed.
The results of this work proved to be essential to have a guide with guidelines of nursing interventions based on scientific evidence, to support the development of food skills of premature newborn and to promote the development of research careers and increase knowledge in this area so important for the future of these infants.
The existence of a mentor guide also allows parents to know better the baby but also to identify signs of instability and stress. Helping parents to become better caregivers and autonomous in the implementation of techniques will promote the babies’ transition to oral feeding.
An algorithm for the preterm infants oral feeding, as represented in the following figure was developed grounded on nurses’ opinion but also in the best available evidence and it is the major contribute of this study to professionals and to parents about oral feeding in newborns premature.
References
Alana W; Timothy M. (2012) - Effects of intrauterine infection or inflammation on fetal lung development: Clinical and Experimental Pharmacology and Physiology. Proceedings of the Australian Physiological Society Symposium: Emerging Leaders in Developmental Physiology Australian. 39. 824–830. doi:
Als, H. (2004)- Prematurity Individualized Developmental Care for Preterm Infants - Centre of Excellence for Early Childhood Development. Encyclopedia on Early Childhood Development.
Als, H. & Gilkerson, L. (1995). - Developmentally Sopportive Care In The Neonatal Intensive Care Init. Nacional Center for Clinical Infant Programs.15(6).
Als, H. [et al.] (2004) - Early experience alters brain function and structure. Pediatrics.113(4) 846–857.
Amaizu, N. [et al] (2008) - Maturation of oral feeding skills in preterm infants. ActaPaediatr. 97(1). 61–67.
Barlow, Steven [et al] (2008) - Respiratory Distress Syndrome Degrades the Fine Structure of the Non-Nutritive Suck In Preterm Infants. Journal of Neonatal Nursing.14(1).9.
Barlow, S. [et al.] (2008)- Synthetic orocutaneous stimulation entrains preterm infants with feeding difficulties to suck. Journal of Perinatology.28. 541-548. [consult. 26 Nov. 2011]. Disponível na internet: <http://web.ebscohost.com/ehost/pdfviewer/pdfviewer?vid=6&hid=11&sid=0a73b7cf-9018-4049-ae49-05eaecd7224e%40sessionmgr12>
Barlow, S. [et al] (2010) - Feeding Skills in the Preterm Infant. The ASHA Leader. [em linha] (June 8,) [Accessed in 22/03/2013]. Available: <http://www.asha.org/Publications/leader/2010/100608/Feeding-Skills-Infant/>
Barlow, S. (2009) - Central pattern generation involved in oral and respiratory control for feeding in the term infant. Current Opinion in Otolaryngology & Head and Neck Surgery.17.187–193.
Bauer, M. [et al] (2009) - Avaliação da estimulação sensório-motora-oral na transição da alimentação enteral para a via oral plena em recém-nascidos pré-termo. Revista Brasileira Saúde Materno Infantil. 9. 429-434.
Bingham, P. [et al.] (2011) - Relationship of behavioral state and tube-feeding to non-nutritive sucking in premature infants. Journal of Neonatal Nursing. 17. 150-157. doi:10.1016/j.jnn.2010.07.02324
Bingham, P. [et al.] (2012) - Relationship of Neonatal Oral Motor Assessment Scale to Feeding Performance of Premature Infants. Journal of Neonatal Nursing. 18(1) 30–36. doi:
Breton, S. & Steinwender, S. (2008) - Timing Introduction and Transition to Oral Feeding in Preterm Infants: Current Trends and Practice. Newborn and infant nursing reviews. 8(3) 155. doi:
Briere, Carrie-Ellen [et al.] (2014) - State of the Science -A Contemporary Review of Feeding Readiness in the Preterm Infant. Continuing Education. J Perinat Neonat Nurs. 28(1)11–58. DOI:
Bu'lock F; Woolridge, M & Baum J. (1990),.- Development of co-ordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants.- Developmental Medicine And Child Neurology.32(8) 669-78. PMID: 2210082; ISSN: 0012-1622.
Cheong, J. & Doyle, L. (2012) - Increasing rates of prematurity and epidemiology of late preterm birth. Journal of Paediatrics and Child Health. 48(9)784–788, DOI: 10.1111/j.1440-1754.2012.02536.x
Crowe, L, Chang, A. & Wallace, K. (2012) - Instruments for assessing readiness to commence suck feeds in preterm infants: effects on time to establish full oral feeding and duration of hospitalization. Cochrane Database of Systematic Reviews. 4. CD005586
Da Costa, S. [et al.] (2010) – The Development of Sucking Patterns in Preterm, Small-for-Gestational Age Infants .Journal of Pediatrics. 157(4) 603-609.
Dodrill, P. (2011) - Feeding Difficulties in Preterm Infants. ICAN. Infant, Child, and Adolescent Nutrition. 3(6) 324-331.doi: 10.1177/1941406411421003
Duffy. F; Als, H. (1988) - Neural plasticity and the effect of a supportive hospital environment on premature newborns. Kavanagh JF, editor. Understanding Mental Retardation: Research Accomplishments and New Frontiers. 179-206.
Finan, D; Barlow, S (1998),.-Intrinsic dynamics and mechano sensory modulation of non nutritive sucking in human infants. Early Human Development. 52. 181-197.ISBN 0 4407378 3
Fucile, S. [et al.] (2011) - Oral and non-oral sensorimotor interventions enhance oral feeding performance in preterm infants. Development Medicine et Child Neurology.53(9).829–835. doi:
Fucile, S; Gisele, G & Lau, C. (2005)- Effect of an oral stimulation program on sucking skill maturation of preterm infants. Developmental Medicine et Child Neurology.47. 158–162.
Fucile, S; Gisele, G & Lau, C. (2002)- Oral stimulation accelerates the transition from tube to oral feeding in preterm infants. Journal of Pediatric.
Goldfield, E. [et al.] (2010) - Premature Infant Swallowing: Patterns of Tongue-Soft Palate - Coordination Based Upon Video fluoroscopy. Infant Behavior Dev.33(2). 209–218. doi:10.1016/j.infbeh.2009.10.001.
Grose, S. (2011)- Feeding, Gavage: Newborn - Transitioning to Oral Feeding. Nursing Practice Council. 20, ICD-996.3511
Horner, S. [et al.] (2014) - Setting the Stage for Successful Oral Feeding- The Impact of Implementing the SOFFI Feeding Program With Medically Fragile NICU Infants. J Perinat Neonat Nurs. 28 (1).59–68 . DOI:
Jeanie L.& Lex W. (2012) - Increasing rates of prematurity and epidemiology of late preterm. Journal of Paediatrics and Child Health. 48. 784-788 doi:10.1111/j.1440-1754.2012.02536.x788 784–birthjpc_2536 784..788© 2012 The Authors Review Article
Lau, C (2006). - Oral feeding in preterm infants. Neo Reviews. Vol. 7.
Lau, C (2012). Development of Oral Feeding Skills in the Preterm Infant. V.R. Preedy (ed.), Handbook of Growth and Growth Monitoring in Health and Disease.499, DOI
Lau C & Schanler R. (1996), - Oral motor function in the neonate. Clinics in Perinatology.23.161–178.
Lau, C; Smith, E; Schanler, R. (2006)- Coordination of suck-swallow and swallow respiration in preterm infants. Acta Pædiatr. 92. 721–727. Stockholm. ISSN 0803-5253
Mathew, O. (1991), - Breathing patterns of preterm infants during bottle feeding: Role of milk flow. Journal of Pediatrics. 119. 960–965.
Mcanulty, G. [et al.]. (2013)- School-age effects of the newborn individualized developmental care and assessment program for preterm infants with intrauterine growth restriction: preliminary findings. BMC Pediatric 13(25) <http://www.biomedcentral.com/1471-2431/13/25>
Mccain, G. [et al.] (2001), - A feeding protocol for healthy preterm infants that shortens time to oral feeding. J Pediatr. 139. 374–379
Medeiros, A. [et al.] (2010).-Caracterização da técnica de transição da alimentação por sonda enteral para seio materno em recém-nascidos prematuros. J Soc Bras Fonoaudiol.23(1)
Pickler, R. (2004), - A Model of Feeding Readiness for Preterm Infants. Neonatal Intensive Care; 17(4) 31–36.
Poore, M [et al.] (2008) - Patterned orocutaneous therapy improves sucking and oral feeding in preterm infants. Acta Paediatr.97(7)920–927. doi:10.111/j.1651-2227.2008.00825.x
Portugal, Instituto Nacional de Estatística: População e Sociedade (INE). (2012). Estatísticas Demográficas INE I.P (Ed.).
Ratynski, N [et al.] (2002) - L’observation du comportement du nouveau-né: une source pertinented’informations médicales - The neonatal behavioral observation: a pertinent source of medical informations. Archives de Pédiatrie. 9.1274 – 1279
Ross, E.& Philbin, k. (2011) - Supporting Oral Feeding in Fragile Infants - An Evidence-Based Method for Quality Bottle-Feedings of Preterm, Ill, and Fragile Infants. Journal Perinatal Neonatal Nurse. 25 (4)349–357. DOI:
Shiao S. (1997) - Comparison of continuous versus intermittent sucking in very-low-birth-weight infants. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 26.313–319.
Stumm, S. [et al.]. (2008), - Respiratory Distress Syndrome Degrades the Fine Structure of the Non-Nutritive Suck In Preterm Infants. J Neonatal Nurs.14 (1) 9–16.
Wolff, H. (1968). The serial organization of sucking in the young infant. Pediatrics 943-956. <http://pediatrics.aappublications.org/content/42/6/943
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
31 July 2016
Article Doi
eBook ISBN
978-1-80296-012-9
Publisher
Future Academy
Volume
13
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-462
Subjects
Health psychology, psychology, health systems, health services, ocial issues, teenager, children's health, teenager health
Cite this article as:
Neto, F., França, A. P., & Cruz, S. (2016). An Algorithm Proposal To Oral Feeding In Premature Infants. In S. Cruz (Ed.), Health & Health Psychology - icH&Hpsy 2016, vol 13. European Proceedings of Social and Behavioural Sciences (pp. 87-98). Future Academy. https://doi.org/10.15405/epsbs.2016.07.02.8

